First aid : Blisters
Blisters are fluid-filled bumps that look like bubbles on the skin. You may develop a blister on your foot when you wear new shoes that rub against your skin or on your hand when you work in the garden without wearing gloves. Home treatment is often all that is needed for this type of blister.
Other types of injuries to the skin that may cause a blister include:
- Burns from exposure to heat, electricity, chemicals, radiation from the sun, or friction.
- Cold injuries from being exposed to cold or freezing temperatures.
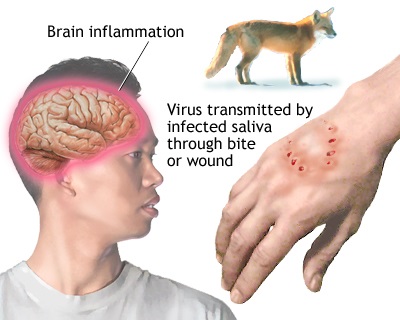
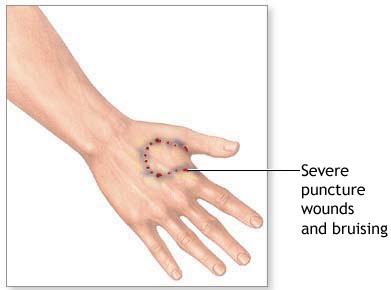
- Some spider bites, such as a bite from a brown recluse spider. Symptoms of a brown recluse spider bite include reddened skin followed by a blister that forms at the bite site, pain and itching, and an open sore with a breakdown of tissue (necrosis) that develops within a few hours to 3 to 4 days following the bite. This sore may take months to heal.
- Pinching the skin forcefully, like when a finger gets caught in a drawer. A blood blister may form if tiny blood vessels are damaged.
Infection can cause either a single blister or clusters of blisters.
- Chickenpox (varicella) is a common contagious illness that is caused by a type of herpes virus. Chickenpox blisters begin as red bumps that turn into blisters and then scab over. It is most contagious from 2 to 3 days before a rash develops until all the blisters have crusted over.
- Shingles , often seen in older adults, is caused by the same virus that causes chickenpox. Shingles blisters look like chickenpox, but they usually develop in a band on one side of the body.
- Hand-foot-and-mouth disease, another type of viral infection, most often occurs in young children. Symptoms include a rash of small sores or blisters that usually appear on the hands and feet and in the mouth.
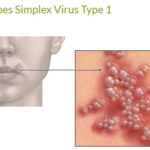
- Cold sores , sometimes called fever blisters, are clusters of small blisters on the lip and outer edge of the mouth. They are caused by the herpes simplex virus. Cold sore-type blisters that develop in the genital area may be caused by a genital herpes infection.
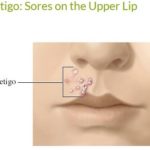
- Impetigo is a bacterial skin infection. Its blisters, which often occur on the face, burst and become crusty (honey-colored crusts).
- Infected hair follicles (folliculitis) cause red, tender areas that turn into blisters at or near the base of strands of hair.
- A scabies infection, which occurs when mites burrow into the skin, may cause tiny, itchy blisters that often occur in a thin line or curved track.
- Bedbugs can cause tiny, itchy blisters anywhere on the body.
 |
 |
 |
 |
 |
 |
Blisters – Home Treatment
Most blisters heal on their own. Home treatment may help decrease pain, prevent infection, and help heal large or broken blisters.

- A small, unbroken blister about the size of a pea, even a blood blister, will usually heal on its own. Use a loose bandage to protect it. Avoid the activity that caused the blister.
- If a small blister is on a weight-bearing area like the bottom of the foot, protect it with a doughnut-shaped moleskin pad. Leave the area over the blister open.
- If a blister is large and painful, it may be best to drain it. Here is a safe method:
- Wipe a needle or straight pin with rubbing alcohol.
- Gently puncture the edge of the blister.
- Press the fluid in the blister toward the hole so it can drain out.
Do not drain a blister of any size if:
- You have a condition such as diabetes, HIV, cancer, or heart disease, because of the risk of infection.
- You think your blister is from a contagious disease, such as chickenpox, because the virus can be spread to another person.
If a blister has torn open, or after you have drained a blister:
- Wash the area with soap and water. Do not use alcohol, iodine, or any other cleanser.
- Don’t remove the flap of skin over a blister unless it’s very dirty or torn or there is pus under it. Gently smooth the flap over the tender skin.
- Apply an antibiotic ointment and a clean bandage. If the skin under the bandage begins to itch or a rash develops, stop using the ointment. The ointment may be causing a skin reaction.
- Change the bandage once a day or anytime it gets wet or dirty. Remove it at night to let the area dry.
Watch for a skin infection while your blister is healing. Signs of infection include:
- Increased pain, swelling, redness, or warmth around the blister.
- Red streaks extending away from the blister.
- Drainage of pus from the blister.
- Fever.
Blisters – Prevention
Some of the most common types of blisters can be prevented.
- To prevent blisters caused by rubbing (friction blisters):
- Avoid wearing shoes that are too tight or that rub your feet. Roomy footwear has a wide toe box with more room for your toes and the ball of your foot. You should be able to wiggle your toes in your shoes. Foot size may vary half a size from the morning to the evening or after a day at work, so purchase shoes at the end of the day when your feet are most swollen.
- Wear gloves to protect your hands when you are doing heavy chores or yard work.
- Avoid contact with any plants or other substances that are known to cause blistery rashes.
- Avoid contact with people who have infections that are known to cause blisters, such as:
- Viral illnesses, including chickenpox, shingles, genital herpes infection, and cold sores.
- Bacterial skin infection (impetigo).
- Scabies mite infection.
First aid video for foot blisters
First aid video for treat the blisters