Hydro colloids
Wouldn’t it be great if you didn’t have to worry about getting scars from your wounds and burns? Wouldn’t it be great if you had hospital style dressings at home? Wouldn’t it be great if you had a wound dressing the made the pain go away? What if I told you that this was all possible, and easy to obtain? All of the above are features of a Hydro colloid. Dressings that, up until recently, were used only in hospitals for burns, minor wounds, and surgery patients.
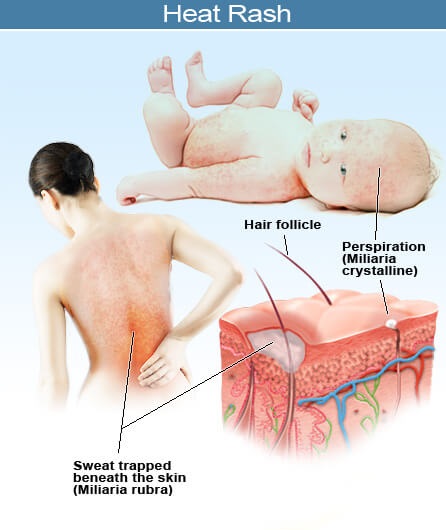
Hydro colloids are a thin dressing that is placed directly over the wound. Although it adheres to your skin, it will not adhere to the wound, which makes removal much less painful. The dressing is covered with a special absorbent material (hydro colloid) that absorbs fluid from the wound, and allows excess fluid to evaporate but at the same time is impermeable to oxygen, water, bacteria and other germs. In this way the hydro colloid creates a moist humid wound environment, which promotes faster healing and helps prevent scarring. Because the wound is moist, no hard scab is formed. Hydro colloids are the most natural way for the body to heal itself, and also the least damaging, as scabs leave scars and can be broken thus opening the body to new infection and damage.
How to use these dressings:
Like with other wound dressings, make sure the wound has been cleaned of any dirt and debris prior to application of the dressing. Because hydro colloids promote moist wound healing, using these dressings on a wound that has not been cleaned is not advised. When cleaning the wound, stick to the basics, like water. Do not use any ointments such as Bacitracin, as it will discourage healing, and the dressing will be rendered ineffective. Harsh cleansers such as hydrogen peroxide should also be avoided.
These dressings are not meant to be used where there is heavy or even moderate bleeding, as they will not stick to the wound as well, and it will delay the healing process to trap the blood in and around the wound. In the case of our burn dressings, Do Not use them on any burn worse than a first degree!! Second and third degree burns are more serious and should be checked out by a doctor. If you are uncertain of the degree of burn, check our burn page, or call a health professional for a second opinion. These dressing should be applied as soon as possible to the wound- if healing, drying or scabbing has already begun then the products will be less effective.
when you use place a hydrocolloid over a wound?
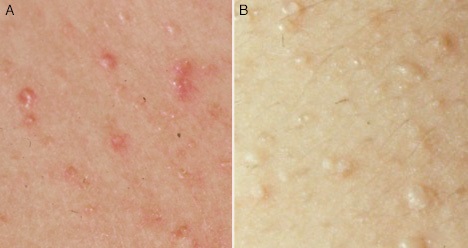
When the dressing is applied to the wound the person with the wound will notice that almost immediately the pain of the wound will lessen or go away. This is because the hydrocolloid material has an anesthetic effect and will help to reconnect the nerve endings that may have been damaged/exposed and are causing the pain. Soon after applying this dressing you may notice a whitish gel starting to form over the wound- This is Normal! This is your body beginning the healing process, and is supposed to happen, there is no need to be alarmed, or worry about an infection. If you have cleaned the wound properly before applying the dressing, and removed any traces of dirt, then you should be fine. If the wound was bleeding at all, you might see a reddish discoloration but this is also nothing to be concerned about.
Hydrocolloids are intended for multi-day use. They can be worn safely for as many days as it takes the hydrocolloid part of the dressing to fill up with fluid (typically 2-5 days). Once the dressing as absorbed as much fluid as it can, it will either fall off – as in the case of burn dressings where the hydrocolloid makes up the entire dressing – or it will need to be removed. If the dressing fills up with fluid, it is time to replace it. This time, unless dirt gets into the wound, you do not need to wash it, as you do not want to disrupt the healing process. If you notice the pad filling up, be sure to carry an additional dressing or two, so you can change it when necessary.
Removing the dressing
This is the part that gives people the most trouble, but it doesn’t have to.
The dressing is designed to remain firmly adhered to your skin (but not the wound), and has a strong adhesive quality on both the hydrocolloid and the film surrounding it. Pulling at this dressing, will cause quite a bit of pain, and can cause the skin to redden and disrupt the wound healing process. To avoid this discomfort, follow these simple directions.
1. Hydrocolloids and the film around them have elastic qualities. You may have noticed this when applying the dressing, the components stretch easily. This is important for the removal of the dressing.
2. Instead of pulling in the opposite direction, which will cause severe pain and skin reddening, pull the ends outwards, in a forward direction away from the hydrocolliod. The purpose is to stretch them like an elastic, or rubber band. While it may pull a little (if the film is stuck to hair), the film and hydrocolloid should lift from the skin pretty easily. The more you stretch it, the easier it will come off. The dressing should not stick to the actual wound.
As mentioned above, the wound generally does not need to be cleaned again, unless dirt enters the wound before a fresh dressing is applied. Occasionally the hydrocolloid will leave some residues behind near the wound. These residues may be gently washed off before the applying the new dressing to continue optimal healing conditions.
Those pesky fraying edges…
These dressing are strong adherents but they are not immune to developing raised edges, which will collect dirt, dust, and other fibers. To keep the dressing neat, carefully trim off any raised edges with a pair of fine, sharp small scissors. The dressing does not need to be removed, and edges can be clipped until you get near the hydrocolloid in the center, or near where the wound exudates (fluid) has extended.
Other important notes about Hydrocolloids:
If you’re changing the dressing more than once a day, or very frequently, you may need a higher strength dressing, and should consult your doctor who may recommend a hydrocolloid paste or powder, and a different solution altogether. Do not use these products (pastes or powders) without consulting a doctor first to make sure they are appropriate.
If your wound is showing signs of possible infection or has already become infected do NOT use these dressings! Their safety has not yet been proven on clinically infected wounds
In a study that involved laceration, abrasion and small operating incision patients, a hydrocolloid dressing was compared with a non-adherent dressing. The results were as follows. Although the healing time was the same for both groups, the patients using the hydrocolloids won out overall. Those using the hydrocolloids experienced less pain, and were able to carry out normal daily activities (such as bathing) without disturbing the wound or the dressings.


.jpg?timestamp=1466788164335)